Why Isn't My Chemotherapy Working?

Is your chemotherapy or cancer treatment plan working in the way you hoped for? This is a question that patients and their loved ones have asked each other during the course of treatment. Unfortunately, when patients ask this question of doctors using the traditional model of cancer treatment, the answer they give is almost always “Let's wait and see.” You need to wait for imaging, wait for blood work, wait and see if the treatment you are getting is actually hitting the correct targets for your specific cancer. Without taking a personalized approach to your specific cancer diagnosis, there will always be potential treatment targets which are missed or overlooked. Over the last two decades, Envita has been perfecting a better approach to cancer treatment by utilizing the highest level of technology and personalization available, summarized in a method we call “N of 1”.
Disclaimer: Individual results will vary. Envita makes no guarantees for outcomes. Each patient case is unique. Please consult your doctor before making any changes to your medical treatment. Not every patient is a candidate for care or achieves these results. Treatments used in this case may not all be FDA approved for the treatment of this condition.
“N of 1” is a reference that means the entire treatment is built on the individual patient's genomics, immunity, causes of cancer, and tumor microenvironment as opposed to standard and outdated clinical trial methodology. The old way of thinking generalizes the larger population without the key details for specific cancer targeting. Large clinical trials may work to study a safety profile of a new medication but not so well for finding exactly what each patient really needs since the data is too broad and undefined. It is important to mention here that the reason we use the word “outdated” is because every patient's cancer is unique and we can see this clearly with the advent of genomics, molecular profiling and biomarkers. Therefore, giving everyone the same treatment based on an algorithm tied to tissue type and location of the cancer is an outdated methodology and one of the reasons so many late stage cancer patients fail treatment in the vast majority of cancer hospitals and centers.
The real issue, however, is that most patients do not understand how their cancer treatment was designed in the first place or know about newer cutting-edge techniques like real-time genomics and others based not on tumor biopsy but circulating tumor cells to take out much of the guess work out of selecting the best treatment agent for each individual patient. The real-time genetic testing allows for a far more accurate method of obtaining tumor genetic information than only using traditional biopsies. Testing biopsies for genetic information can be an incomplete method since the tumor inside the patient's body has often mutated even further before the analysis can be completed and contains genetic information from only the primary site. In the current model of cancer treatment used by most hospitals like Mayo Clinic, MD Anderson, and Sloan Kettering as well as the rest of the major cancer centers in America, treatment is based on the accumulated data from clinical trials and the doctors create drug regimens like algorithms based on this data and tumor board discussions. The problem is that they are basing your treatment on these other people's data and not your own!
Disclaimer: Individual results will vary. Envita makes no guarantees for outcomes. Each patient case is unique. Please consult your doctor before making any changes to your medical treatment. Not every patient is a candidate for care or achieves these results. Treatments used in this case may not all be FDA approved for the treatment of this condition.
It has been well established by increased genetic analysis of various cancers that each case of cancer is unique and that there are no two patients which would have identical targets for treatment. The traditional model of cancer treatment uses a very broad set of criteria in which to divide treatment for patients based on a fixed algorithm. This cancer-type based algorithm is largely outdated as the approach lacks any real personalization or taking into account more detailed biometrics that can be collected now from the patient. Everyone deserves to be looked at as an individual for their personal medical treatment, what we call “N of 1.” That's why our team specializes in personalized targeting for difficult to treat and late-stage cancers.
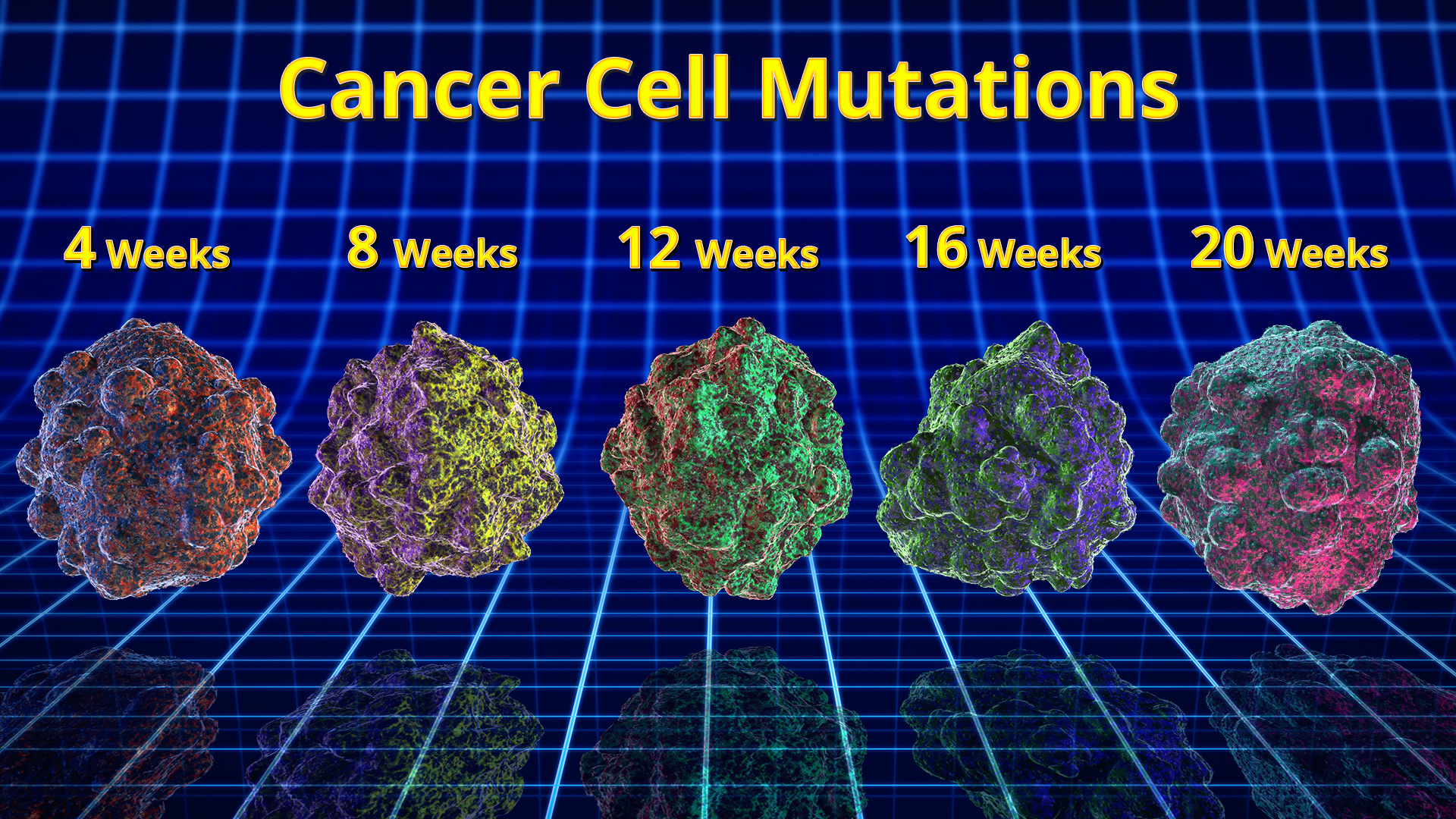
Algorithmic or traditional protocols for cancer therapy seem to work best in the early stages, such as Stage 1 or even Stage 0. In the early stages, surgery accomplishes 90% of the work and radiation or chemotherapy serves a more prophylactic purpose. Early stage cancers are usually far less complex and are thus easier to treat than late-stage cancer which can have essentially many moving parts. Many decades ago, when the clinical trials first began, the theory was that cancer was essentially one disease that could be separated into categories based on factors like tissue type and stage. We now know today that cancer is not at all like an infectious or other common diseases. Cancer arises from accumulated genetic mutations that cause the cells to multiply rampantly. Not only that, but receiving the wrong chemotherapy promotes the accumulation of more and more mutations over time, making the cancer grow faster and become more resilient; one strain of cancer can even diversify and become multiple genetic variants with difficult to target cancerous stem cells! Often, the cancer can even suppress the host's own immune system which regularly destroys abnormal cells which are formed in the body every day, a beneficial mutation for the cancer, but disastrous for the patient.
Unfortunately, in the history of medicine, there is a precedent for the slow absorption and incorporation of new scientific evidence and technology. Frequently, doctors themselves put up barriers to new information, new techniques, or more importantly, entirely new modes of thought. It often takes years or even decades of a technique being used outside of the conventional treatment model for it to catch on and become accepted by the larger medical community. The strange part here is that if you attended any major oncology conference anywhere in the world the discussion is usually about genomics, immunotherapy and targeting, yet the predominate practice is same old protocols with minor modifications. The side-effect of this unwillingness to accept change is that lives are degraded or lost entirely by lack of access to medicine that could potentially help them today. Our team focuses on bring the best and latest technology to our patient as soon as possible.
The cookbook style protocol for treating cancer has made some progress towards reducing the risk of death from cancer. The vast majority of this progress, however, has come from early detection and early treatment protocols. For patients with late stage, or complicated cancer, there remains a lot to be desired in terms of an effective approach. For these patients, the goal has largely been to manage rather than eradicate the cancer. Our years of experience has proven that you must do both simultaneously and with a highly personalized approach to each individual patient.
It is important to remember that in the standard cancer treatment regimen, the informing data is built upon pre-existing clinical trial data and does not incorporate any new information from the actual patient beyond just a few pre-determined and broad factors such as whether they are pre- or postmenopausal or have received endocrine therapy. The patient's molecular profile and the genetic expression of their cancer is often not considered. When it comes to dosing, the Maximum Therapeutic Dose (MTD) is often considered as a benchmark, especially for late-stage or difficult to treat cancers. It is generally known that the side-effects are extremely high for such an approach to chemotherapy, and yet there is evidence to suggest that using very high doses of these toxic medicines actually promotes resistance in the surviving cancer cells making them become less sensitive to future treatment as a result.
Disclaimer: Individual results will vary. Envita makes no guarantees for outcomes. Each patient case is unique. Please consult your doctor before making any changes to your medical treatment. Not every patient is a candidate for care or achieves these results. Treatments used in this case may not all be FDA approved for the treatment of this condition.
Instead our medical team advocates for a treatment regimen known as Genetically Targeted Fractionated Chemotherapy which utilizes metronomic dosing. Envita published extensively on this treatment modality in the 2015 Journal of Cancer Therapy titled Novel Approach to Chemotherapy and Administration Selection with Metronomic/Fractionated Dosing. As opposed to MTD (maximum therapeutic dosing), which consists of administering a very high dose of chemotherapy at once, metronomic dosing requires low, and in Envita Clinic's case genetically targeted, doses equally spaced out over a longer period. This allows the therapy to hit many more targets at once and reduces side effects at the same time. There are several advantages to using this technique, primarily in avoiding some of the more toxic side effects such as weight loss, nausea, and wasting. There have already been some preliminary experiments that show the effectiveness of metronomic dosing equals or even exceeds the results of conventional dosing in some cases[1,2].
There are a number of reasons why metronomic dosing is effective. Drugs chosen for this procedure typically target angiogenesis, or the formation of new blood vessels and a process that both feeds tumor growth and allows for metastatic cells to break off into the bloodstream to colonize new parts of the body other than the primary tumor. Obstructing tumor vasculature starves cancer cells of nutrients and oxygen, slowing the progress of the disease. As Klement mentions in some of the preliminary research into metronomic dosing, the lower drug doses delays or prevents the cancer from acquiring drug resistance and allows for several drugs to be used in conjunction that would otherwise be too toxic to tolerate at the MTD2. These are major benefits to this approach at delivering chemotherapy, especially for late-stage or complex cancers. Although the inhibition of angiogenesis slows cancer growth, there has been more interesting work also done in terms of specific targeting of cancer cells based upon certain genetic properties that can be revealed by detailed analysis of an individual's specific form of cancer. For example, Gemcitabine and a related drug still under heavy testing, have shown antitumor activity on several different kinds of cancer while applied in metronomic testing. Gemcitabine functions by blocking DNA synthesis in a process that involves it being incorporated into the cancer cell's DNA structure itself[3-6], but these are only two such drugs at the disposal of physician's today[7,8].
Pathologists and oncologists today have the opportunity to provide more precise and tailored cancer treatments than ever before, however it does require the combination of complex molecular tests, new treatment methods and the existing body of clinical evidence. It is a time consuming and labor intensive exercise of technology and application of cutting-edge medical knowledge that many hospitals do not bother with, but is the best and only way to treat based on our clinical experience. There is a lot more to find out about the kinds of unique and personalized treatment regimens we have available. Even if you've been told that your options are limited, there's always room for a second opinion. Give us a call at 1-866-830-4576, our medical staff is well trained and able to answer any questions you might have.